
Proper care of cleaning equipment is critical in reducing the spread of infectious disease and maintaining hospital hygiene standards.
Every year, 165,000 healthcare-associated infections (HAIs) occur in Australian hospitals. These lead to over 380,000 additional hospital bed days and millions in healthcare costs. HAIs remain a major risk to patient health, yet many are preventable through effective cleaning practices.
Hospital teams must go beyond disinfecting equipment surfaces and medical instruments. They should also focus on the cleaning of equipment such as mops, buckets, and other machines used in the cleaning process. If not effectively cleaned, these items can become sources of contamination, spreading bacteria, body fluids, and recycled matter across high-touch surfaces.
Using the proper cleaning methods, appropriate agents, and personal protective equipment are all essential components of safe and compliant sanitation tasks in a hospital setting.
Healthcare facilities are in constant flux. Patients move in and out of rooms, visitors come and go, medical workers circulate through buildings and cleaning staff make rounds through all areas of the facility.
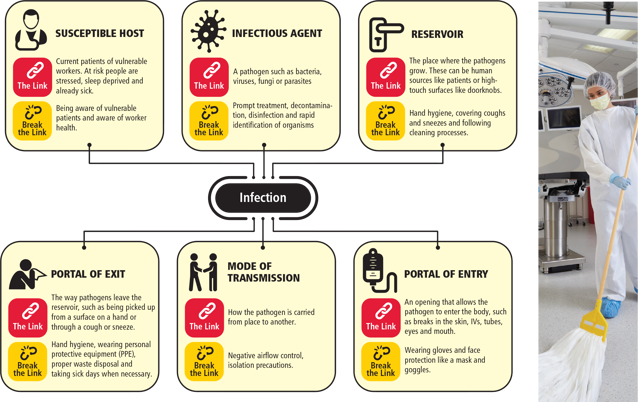
All of this movement makes it easier for infections to spread from place to place and person to person. The chain of infection follows a familiar pattern:
Susceptible host: Current patients of vulnerable workers. At risk people are stressed, sleep deprived and already sick.
Infectious agent: A pathogen such as bacteria, viruses, fungi or parasites.
Reservoir: The place where the pathogens grow. These can be human sources like patients or high-touch surfaces like doorknobs.
Portal of exit: The way pathogens leave the reservoir, such as being picked up from a surface on a hand or through a cough or sneeze.
Mode of transmission: How the pathogen is carried from place to another.
Portal of entry: An opening that allows the pathogen to enter the body, such as breaks in the skin, IVs, tubes, eyes and mouth.
Breaking the chain of infection requires key interventions at each stage of the cycle
Susceptible host: Being aware of vulnerable patients and aware of worker health.
Infectious agent: Prompt treatment, decontamination, disinfection and rapid identification of organisms.
Reservoir: Hand hygiene, covering coughs and sneezes and following cleaning processes.
Portal of exit: Hand hygiene, wearing personal protective equipment (PPE), proper waste disposal and taking sick days when necessary.
Mode of transmission: Negative airflow control, isolation precautions.
Portal of entry: Wearing gloves and face protection like a mask and goggles.
At the reservoir and portal of exit stages, adequately trained staff are responsible for breaking the chain of infection. Cleaning equipment—if not maintained—can store and transfer pathogens between other surfaces, patients, or staff. Items such as wipes, cloths, and reusable instruments used across different areas must be managed carefully.
If used on food contact surfaces or around hot water areas like sinks or tables, cross-contamination can occur. This makes maintenance and safe storage part of the broader infection control strategy, helping hospitals across Australia minimise risks and uphold safety standards.
If not properly maintained, cleaning equipment can become a source of cross-contamination in healthcare environments. When used in areas exposed to pathogens, tools like mops, cloths, and other devices can transfer bacteria to new surfaces. For example, placing a used mop directly into a solution without rinsing may contaminate the solution itself.
To support food safety, infection control, and effective hospital hygiene, follow the steps below to clean and store hospital cleaning equipment correctly.
Start the process by rinsing all used equipment with clean water. This helps remove protein residues, grease, and visible food waste before disinfection. Rinsing also improves the action of cleaning agents in later steps.
Select cleaning products suitable for the item and application. Always refer to the manufacturer’s instructions for approved cleaning agents, whether using manual cleaning or mechanical cleaning methods. Some products may require organic acids, quaternary ammonium compounds, or hydrogen peroxide to destroy microorganisms effectively.
Use warm water or steam, depending on the equipment’s tolerance to temperature, and always follow the recommended contact time for maximum effectiveness.
Use detergent and brushes where needed to remove build up on equipment, especially in crevices or around wheels. Items like buckets, mop handles, and reusable utensils should be thoroughly washed to prevent the spread of contaminants across high-volume hospital areas.
After washing, rinse again with clean water to remove any residual chemicals. Equipment should then be allowed to air dry completely or wiped with a paper towel. Tools that are not fully dry before storage can develop mould or bacteria, posing additional infection risks.
Store items off the floor and away from food contact surfaces. Designated storage areas should allow airflow to support drying and reduce humidity. For better hygiene, separate storage zones by cleaning task or room use (e.g. toilets, kitchens, patient rooms).
Maintain records of cleaning schedules and tool maintenance to monitor time required and support audit requirements in line with hospital protocols.
Only trained cleaners or adequately trained personnel should be responsible for cleaning and maintaining hospital equipment. Staff must understand the correct process, temperature ranges, and chemical sanitisers needed for various tools. Provide further information and ongoing training to keep teams updated on evolving safety standards.
Any equipment that comes in contact with pathogen reservoirs - surfaces like floors and door handles - should be cleaned after each use. For example, cleaning clothes should be laundered under high heat to kill bacteria and similar pathogens. Many healthcare facilities are switching to disposable microfibre systems to reduce the risks associated with multi-use products.
Wet mops are a common source of infection. Staff members may clean an area of the floor and then accidentally touch a damp part of the mop, potentially spreading pathogens to their hands and clothes. Professional microfibre mop kits can eliminate the need to liquid cleaning chemicals.
In addition, switching biohazard spill mops further reduces the risk of spreading pathogens. Unlike regular mops, innovative spill mop pads are designed to absorb bodily fluids and turn them into a gel to prevent dripping. The entire mop head can then be disposed of in a biohazard receptacle.
Cleaning equipment should always be stored in dry areas away from patients and other people. Limiting access to cleaning supplies ensures that only authorised staff members use them.
Storing cleaning supplies in designated caddies keeps everything separated. For instance, cleaning clothes should never come in contact with mopping equipment. Using racks and shelves to keep supplies apart reduces the chance that pathogens will move from one item to another.
Staff members should maintain up-to-date inventory lists for each supply closet. Expired products should be removed promptly. In addition, the supply closet itself should be cleaned regularly. For example, if products drip on the floor, the spill should be cleaned immediately.
Breaking the chain of infection with proper cleaning procedures helps keep patients safe and reduces unnecessary healthcare costs. Maintaining cleaning equipment with the latest best practices can stop the spread of HAIs.
To learn more about the latest innovations in cleaning solutions, check out what Rubbermaid Commercial Products has to offer.